What Is Skin Cancer?
Skin cancer is characterized by the uncontrolled growth of cells in the skin. It has been estimated that 1 in 5 Americans will develop some form of skin cancer during their lifetime. Although skin cancer is rare in childhood, sun exposure in this period has been linked to an increased risk of developing skin cancer in the future. Therefore, preventing excess sun exposure in your children will decrease their risks of developing skin cancer in the future.
There are three types of skin cancer:
- Basal cell carcinoma is the most common type of skin cancer accounting for approximately 75% of all skin cancer. It grows slowly and rarely occurs in children.
- Squamous cell carcinoma accounts for 20% of skin cancer and is more aggressive than basal cell carcinoma, but less aggressive than melanoma. It also rarely occurs in kids.
- Melanoma is the most aggressive form of skin cancer. It arises from pigment-producing cells called melanocytes (the cells that allow you to tan). Therefore, most melanoma begins as a mole. It accounts for 4% of all skin cancer, but causes 79% of all deaths from skin cancer. Approximately 300 cases of melanoma arise in children each year.
In adults, basal cell carcinoma and squamous cell carcinoma represent more than 1 million cases each year, but thankfully they are rare in children. This makes melanoma the most worrisome form of skin cancer for parents to watch out for.
What Are Moles?
Moles, or “nevi,” are skin growths made up of groups of pigment-producing cells, called melanocytes. They are usually brown or black in color. Most moles are benign and cause no problems over a lifetime. Most are acquired “fresh,” between ages 2 and early adulthood. Some moles are present at birth or soon after. These are called congenital moles. Moles can turn into melanoma and that is why it is important to check your child’s moles regularly.
Who Gets Melanoma?
It is important to identify children who are at higher risks of developing melanoma than the general population. The following are characteristics of a person at high risk for developing melanoma:
- Family history of melanoma
- Light skin/red hair/light-colored eyes
- Having more than 50 moles
- Having a giant birthmark or a giant mole
- Having been previously diagnosed with atypical moles
The environment also plays an important role in increasing melanoma risks. The following are environmental factors that increase these risks:
- Excess or chronic sun exposure especially early in life.
- History of blistering sunburns
- Impaired immune system such as having a disease with immune deficiencies like HIV infection or using immunosuppressant drugs like in organ transplant patients
- History of cancer or chemotherapy
How do I Prevent Skin Cancer in My Child?
Sun Protection: Because sun exposure is the most important risk factor and is the only one that is modifiable, skin cancer prevention almost solely depends on sun protection. The following are guidelines from the American Academy of Dermatology for sun protection in order of decreasing importance:
- Avoid the sun between 10 am and 4 pm, the period of the day when sunrays are strongest. Seek shade whenever possible. Keep infants under 6 months out of direct sunlight. And pay attention to UV Index that is reported daily in newspaper, and on TV and radio. It is on a scale of 1 to 11+, the higher the UV Index, the less time it takes to burn.
- Protective clothing – Choose clothes that are tightly woven and, ideally, SPF rated. A general rule of thumb is to hold the clothing up to a source of light and see how much light shines through. A hat should cover both the face and the back of the neck. Wide-brim hats are better than baseball caps. Visors offer little or no sun protection. Sunglasses that protect against UVA and UVB are important in protecting the eyes from sun damage.
- Sunscreen use
- Choosing an effective sunscreen:
- Sun Protection Factor (SPF) – Pick an SPF of 30 or higher. The higher the SPF, the greater the protection from sunburn caused mostly by UVB rays, not UVA. Also, the higher SPF does not increase the length of time for sun exposure.
- UVA protection – Most sunscreens protect against UVB, but not UVA. UVA has a longer wavelength, less energy, but is more mutagenic (i.e. cancer-causing) than UVB. Products that contain Oxobenzone or Avobenzone (Parsol) can block UVA, but may break down under the sun and thus only offers no more than 4 hours of UVA protection. Mexoryl is a newer addition to sunscreen ingredients that does not break down in the sun. Another new ingredient, Helioplex, helps stabilize Parsol and allows up to 6 hours of UVA protection. Look for these ingredients in your sunscreen or the AAD SEAL OF RECOGNITION on sunscreen products to ensure protection against UVA.
- Hypoallergenic sunscreen – Most allergic reactions against sunscreen are caused by para-aminobenzoid acid (PABA). If your child has a reaction against sunscreen, try products that do not contain PABA, dyes or perfumes. Also, sunscreens containing titanium dioxide or zinc dioxide provide physical block that reflects both UVA and UVB and has no chemical ingredients suitable for those with prior reactions to sunscreen.
- Non-comedogenic sunscreen – For oily skin, try products that are labeled with “won’t clog pores” or “non-comedogenic” to reduce acne caused by sunscreen.
- Lip sunscreen – It is also important to protect your lips from the sun! Choose a lip balm with SPF 15 or higher.
- New advances in sunscreen technology – Scientists are coming up with sunscreen containing vitamins C and E, which help boost the skin’s defenses against UV damage. There is also a sunscreen “pill,” called Heliocare, that can offer up to three hours of protection. These are currently meant to supplement sunscreens and not to replace them.
- Application:
- Use a generous amount! Generally, an ounce (enough to fill up a shot glass) is used to cover the entire body surface area. If you use less, you will risk decreasing the protection from SPF.
- Apply at least 30 minutes before sun exposure
- Reapply every 2 hours and after swimming and sweating
- Apply sunscreen every time your child goes out in the sun, even if it is cloudy!
*Remember, do NOT use sunscreen as a reason to stay out in the sun longer!
- Choosing an effective sunscreen:
- Avoid tanning beds/booths – remember there is NO safe way to tan because a tan is the first sign of sun damage.
Skin Exam: Along with the practice of sun protection, it is important to do a regular self-skin exam and to have your physician perform a complete skin examination at least once a year. The top of the ears, the forearms, the back of the neck and the back of the legs are especially important to examine. Don’t forget the webs of the fingers, the scalps and the palms and soles. Familiarize yourself with the pattern of moles, freckles and birthmarks on your child’s skin. The mnemonic ABCDE is helpful in deciding if a mole or a birthmark is suspicious:

Asymmetry – one half of the mole looks different from the other half
 Border – the edges of the mole are irregular or not smooth
Border – the edges of the mole are irregular or not smooth
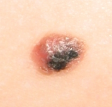 Color – there is more than one color in the mole
Color – there is more than one color in the mole
 Diameter – the mole is larger than 6 mm in diameter
Diameter – the mole is larger than 6 mm in diameter
Evolution – changes such as a sudden increase or decrease in size, bleeding, itching, or color changes in a mole
Consult with your child’s doctor if a mole looks suspicious or if you notice any changes in it. For more information please visit the American Academy of Dermatology at www.aad.org or the U.S. Environmental Protection Agency at www.epa.gov/sunwise.
References:
- Skin Cancer Facts. American Academy of Dermatology.
- Krakowski A, Krakowski F. Golfers who S.L.I.C.E. Reduce Skin Cancer Risk.
- Protecting Your Child from the Sun. American Academy of Pediatrics.
- Schaffer J. Pigmented Lesions in Children: When to Worry. Current Opinion in Pediatrics 2007. 19:430-440.
- Skin Cancer. Department of Dermatology, UvaHealth.com
- Sunscreen Use in Children May Lower Risks of Developing Future Skin Cancer. American Academy of Dermatology.
- Vidimos A. Pediatric Melanoma: what you should know before taking your child out in the sun. PARENTGUIDE News. July 2007.