Heart Modeling

Pediatric heart model (size of a plum) printed in tissue-like material (Tissue Matrix and Agilus 30) on the Stratasys J750TM Digital AnatomyTM 3D Printer).
Nearly one out of every 100 newborns in the United States is born with a heart defect. As medicine has evolved over the recent decades, with the advent of technology such as high-resolution cardiac magnetic resonance imaging (MRI) and cardiac computed tomography (CT) scanning, our ability to examine and understand a child’s heart has vastly improved.
Rady Children’s was the first hospital in San Diego with a 3D heart modeling program, under the direction of Sanjeet Hegde, M.D. P.h.D., and Dr. John J. Lamberti. Dr. Hegde utilized cardiac CT and MRI scans with a special software program to generate a digital dataset. The file was then to a 3D printer, which printed out physical models of patient hearts. The very first heart created in this manner was at the request of a patient’s mother and father.
At Rady Children’s Heart Institute, led by cardiac surgeon John Nigro, M.D., we have continued using 3D models of congenital heart defects to plan complex heart surgeries. The models are also a powerful education tool for patients and families, as the physician can go from evaluating an image of a patient’s heart on a screen to holding a lifelike model of it in his hands.
Orthopedic 3D Printing
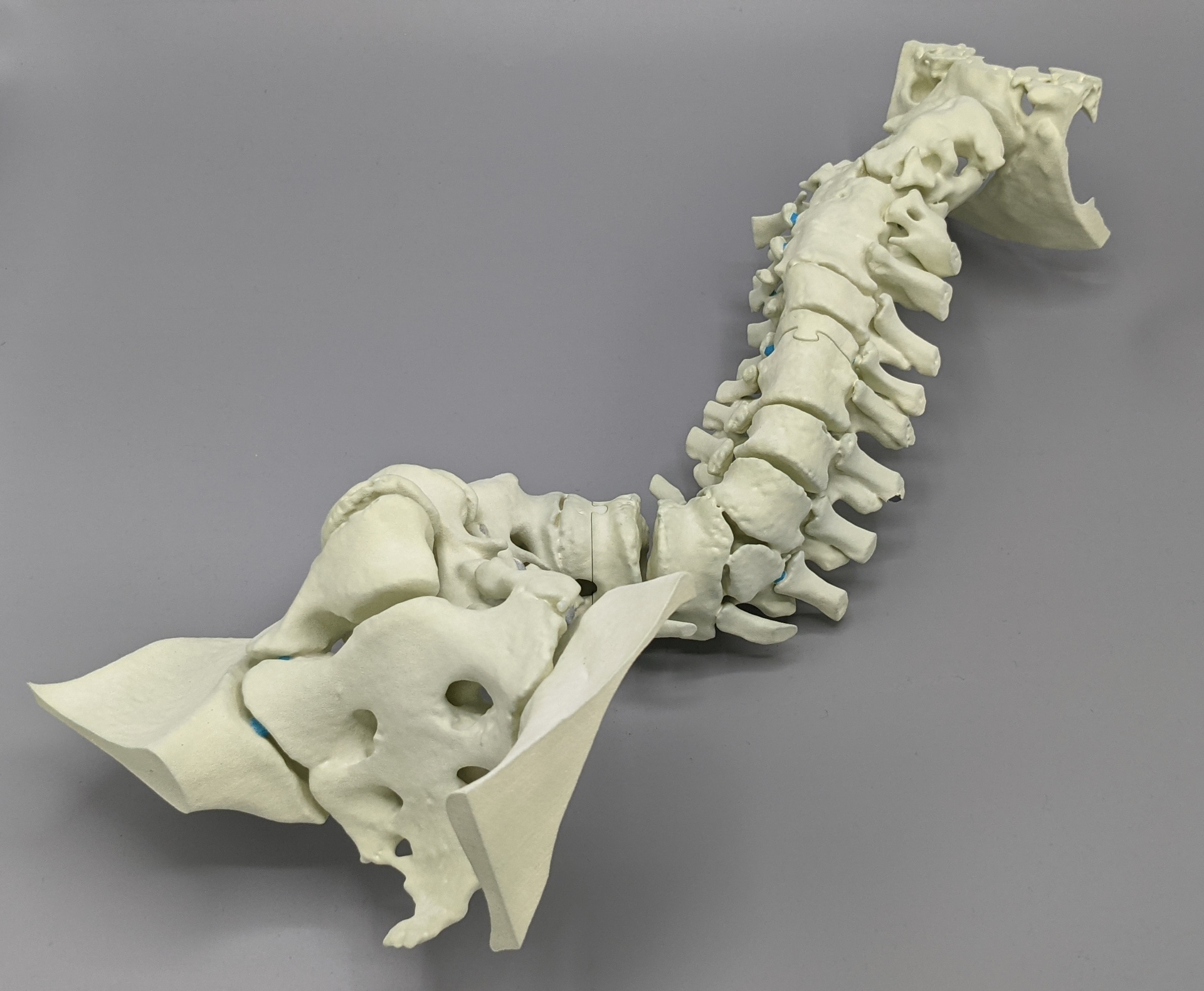 In 2015, the Orthopedics & Scoliosis Center at Rady Children’s purchased a material extrusion 3D printer – remarkably similar to the 3D printers seen at libraries, schools, and possibly your own garage! The use of the 3D printer expanded in 2016 due to a collaboration with UC San Diego. Robert Sah MD PhD, Director of the Cartilage Tissue Engineering (CTE) Lab at UC San Diego, developed a course within the bioengineering undergraduate curriculum that included students producing a 3D printed human spine model using two dissimilar materials.
In 2015, the Orthopedics & Scoliosis Center at Rady Children’s purchased a material extrusion 3D printer – remarkably similar to the 3D printers seen at libraries, schools, and possibly your own garage! The use of the 3D printer expanded in 2016 due to a collaboration with UC San Diego. Robert Sah MD PhD, Director of the Cartilage Tissue Engineering (CTE) Lab at UC San Diego, developed a course within the bioengineering undergraduate curriculum that included students producing a 3D printed human spine model using two dissimilar materials.
In collaboration with Peter Newton, M.D., the CTE lab developed a 3D printing protocol that enabled material properties of diverse types of bone tissue. Surgeon Salil Upasani, M.D., and researcher Lilia Cherkasskiy, Ph.D., investigated the use of 3D prints as pre-operative planning tools for a specific diagnosis (slipped capital femoral epiphysis) and learned that performing “mock” surgery first using the prints lead to 45 minutes decreased surgical time and 50% less fluoroscopy usage.[1] Jason Caffrey, Ph.D., worked with Dr. Upasani to develop a 3D model of the pelvis that mimicked cartilage within the hip joint. [2]
Currently, our Orthopedics program continues to leverage 3D printing for surgical support, medical education, and fundamental, benchtop research.
Software and Virtual Reality
 In late 2019, the 3DI Lab expanded its efforts and began developing software for the hospital with the goal of assisting doctors and surgeons, as well as patients and their families. Since then, the 3DI Lab has produced a wide array of software programs, including Media2DICOM: a tool for converting and encapsulating media files as DICOMS. The 3DI Lab continues to monitor new and emerging innovations for application within the healthcare space, including mixed reality.
In late 2019, the 3DI Lab expanded its efforts and began developing software for the hospital with the goal of assisting doctors and surgeons, as well as patients and their families. Since then, the 3DI Lab has produced a wide array of software programs, including Media2DICOM: a tool for converting and encapsulating media files as DICOMS. The 3DI Lab continues to monitor new and emerging innovations for application within the healthcare space, including mixed reality.
3D Printing for COVID-19 Response
Following the initial reports of COVID-19 reaching the United States, the Helen and Will Webster 3D Innovations Lab engaged in several internal and external initiatives to address various needs arising from the pandemic. The 3DI Lab collaborated with community partners to produce swabs, reusable face shields, and ventilator splitters.
The Webster Foundation 3DI Lab developed the following during early pandemic response:
- 260,000 NP swabs via 3D printing with the San Diego COVID-19 Research Enterprise Network (SCREEN)
- 5,000 reusable face shields via 3D printing and laser cutting for staff and community first responders
- 5,000 “ear savers” for staff
- 3D printed ventilator splitters*
- In-house 3D software to facilitate planning for patient surges
*The ventilator splitters, while developed and produced, were not deployed due to adequate coverage of available resources. However, the files were shared with various other institutions overseas during the “Delta” surge.
References
- Cherkasskiy, L., Caffrey, J. P., Szewczyk, A. F., Cory, E., Bomar, J. D., Farnsworth, C. L., Jeffords, M., Wenger, D. R., Sah, R. L., & Upasani, V. V. (2017). Patient-specific 3D models aid planning for triplane proximal femoral osteotomy in slipped capital femoral epiphysis. Journal of children’s orthopaedics, 11(2), 147–153.
- Caffrey, J. P., Jeffords, M. E., Farnsworth, C. L., Bomar, J. D., & Upasani, V. V. (2019). Comparison of 3 Pediatric Pelvic Osteotomies for Acetabular Dysplasia Using Patient-specific 3D-printed Models. Journal of pediatric orthopedics, 39(3), e159–e164.
- Valdovino, A., Ryan, J., Gholami, P., Bomar, J. D., & Upasani, V. V. (2021). Proximal Femur Osteotomy Guided with Patient-Specific 3D Print Technology: A Case Report. JBJS case connector, 11(3).