What is scoliosis?

Figure 1 Figure 2
Scoliosis is an abnormal curvature of the spine. The normal spine, when viewed from behind has no visible curve. When viewed from the side there will be a slight round back in the upper back and a mild swayback in the lower back. These curvatures of the spine are normal. When scoliosis develops, when viewed from the back, a curvature to the right or left will be seen (Figure 1). Associated with the abnormal curvature, there is also twisting of the spine. This twisting results in asymmetry of the rib cage. When viewed from the back a prominence of the ribs will be visible on the side of the curve.
Scoliosis may develop in one or more areas of the spine. Additionally, the curve patterns in scoliosis vary from short single curves to large double or triple curves (Figure 2).
What causes scoliosis?

Figure 3a – Congenital Scoliosis
There are several causes of scoliosis. In some cases it results from an abnormal development of the bones in the spine. This is called congenital scoliosis and is present from the time of birth, although it may not be recognized until the deformity increases with growth. The primary sources of the deformity in this case are the abnormally shaped bones or asymmetrically fused bones in the spine that do not grow properly (Figure 3a).

Figure 3b – Neuromuscular Scoliosis
Another cause for scoliosis is poor neurologic or muscular control of the spine. In these circumstances, support from the muscles of the back is insufficient to maintain an erect spinal position. This type of neuromuscular scoliosis is seen in conditions such as cerebral palsy, spina bifida, muscular dystrophy, etc (Figure 3b).

Figure 3c
The most common cause for scoliosis in children and adolescents, however, results from unknown causes. When there is no underlying abnormality of the spine or of the neuromuscular system, the scoliosis is considered to be idiopathic (Figure 3c).
Much investigation has gone into looking for the cause of scoliosis in these otherwise normal children, and to date no clear cause has been identified. There does appear to be an increased incidence of scoliosis within a family, suggesting some genetic influence. Thus, scoliosis may develop due to congenital, neuromuscular or unknown causes.
What are the consequences of scoliosis?
The deformity of the spine, in cases of scoliosis, tends to increase with increasing growth of the spine. There are cases, however, in which no progression of the deformity occurs or the increasing size of the deformity is minimal. The shape of the body is altered depending on the scoliosis curve pattern. Concern develops in cases when the deformity is progressive. With large curves, trunk and chest deformity develop to a degree that ultimately inhibits normal lung and heart function. For these reasons, treatment of scoliosis is recommended when a progressive curvature is detected.
How is scoliosis assessed?
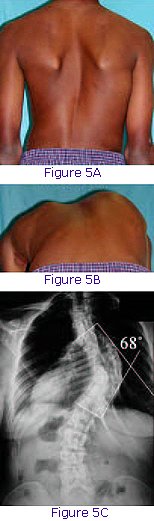 The diagnosis of scoliosis is made by examining the shape of the back and trunk. As scoliosis progresses, a difference in the height of the shoulders may develop, as well as an asymmetry of the waistline and contour of the back (Figure 5a). Because of the rotational changes in the spine with the development of scoliosis, prominence of the ribs occurs. This can be seen most readily by examining the patient from behind when bent forward at the hips (Figure 5b). This forward bending test (Adam’s test) is used in screening patients for scoliosis. In many states, a scoliosis school screening program exists in which all children are examined for back and rib asymmetry.
The diagnosis of scoliosis is made by examining the shape of the back and trunk. As scoliosis progresses, a difference in the height of the shoulders may develop, as well as an asymmetry of the waistline and contour of the back (Figure 5a). Because of the rotational changes in the spine with the development of scoliosis, prominence of the ribs occurs. This can be seen most readily by examining the patient from behind when bent forward at the hips (Figure 5b). This forward bending test (Adam’s test) is used in screening patients for scoliosis. In many states, a scoliosis school screening program exists in which all children are examined for back and rib asymmetry.
When a rib prominence is noted, a standing radiograph of the spine is recommended. The X-ray evaluation of the spine is made to determine the magnitude and pattern of spinal curvature. The angulation (measured in degrees) between the most tilted vertebrae is determined using the Cobb angle method (Figure 5c). It is this measure of scoliosis on which treatment recommendations are based.
In addition to the degree of scoliosis, it is important to assess the skeletal maturity of the patient. It is known that the risk of the curve enlarging is related to the amount of growth remaining in the skeleton and spine. This can be assessed in several ways. The first is a radiographic measure of the maturity of the skeleton, done by analyzing the growth centers of the pelvic bone. The Risser sign is a marker for skeletal maturity, which can be followed on the pelvic X-ray to help predict whether or not growth is expected to continue.
Other measures of remaining growth relate to the changes of puberty that can be assessed in both boys and girls. An additional helpful time point in girls relates to the onset of menstrual periods. The beginning of menstrual period suggests 1½ to 2 years of remaining spinal growth. It is largely these two facts, an estimate of the remaining spinal growth and the magnitude of the spinal curvature, which are used to predict the potential for scoliosis progression. The underlying cause of the scoliosis also plays a significant role in determining the likelihood of progression and need for treatment. It is recommended that a physician with expertise be involved in the care of a patient with scoliosis when the Cobb angle is greater than 15°.
How is scoliosis treated?
The options for treating scoliosis include observation, the use of a brace (orthosis) or surgery. Currently, there is no evidence that exercise or spinal manipulation have a positive effect on preventing the progression of scoliosis.
The treatment of congenital scoliosis initially is observation by checking X-rays of the spine periodically. If increasing curvature is appreciated on serial examinations, surgery may be required to prevent the curve from increasing in size. Bracing is indicated in very few patients with congenital scoliosis. The surgical treatment for such cases is a spinal fusion, which limits the growth of the spine and prevents progression of the curve.
The indications for brace treatment in neuromuscular causes of scoliosis are variable. In many cases the brace is helpful to maintain sitting posture in patients who are unable to walk. The ultimate progression of the curvature may be delayed only slightly. In many neuromuscular conditions curve progression develops despite brace wear. The benefit of bracing in these circumstances is primarily in helping sitting balance. Surgical indications in neuromuscular scoliosis vary depending on the underlying diagnosis, pulmonary status, curve pattern, and magnitude.
Idiopathic scoliosis is treated with a brace in those patients who have curves that are progressing to greater than 25–30° and are thought to have substantial growth remaining.
How does bracing help?
Braces have been used for decades to attempt to limit scoliosis progression, however the true benefit of scoliosis bracing is unclear. For this reason, we have joined a National Institutes of Health-funded randomized clinical trial of bracing. Patients who meet the inclusion criteria for this study will be offer the opportunity to help us understand the true benefit of brace wear for adolescent idiopathic scoliosis.
A brace used to control scoliosis is designed to apply external pressures to the trunk and pelvis, improving the alignment of the spine and allowing straighter growth of the spine (Figure 6a, b). Bracing of scoliosis is not helpful in patients who have completed or nearly completed their spinal growth. Bracing is, therefore, indicated for patients with idiopathic scoliosis with curves between 25–45° with greater than six months of skeletal growth remaining.
There are several types of orthoses or braces available (Figure 7a, b, c). All of the braces attempt to straighten the spine and are most effective if worn full time. The brace is made to fit intimately the patient’s trunk, providing pressure against the pelvis and rib cage to reduce the deformity. A brace maker (orthotist) is used to fit and adjust the brace accordingly. Initial brace wear may be uncomfortable, and a period of time is required to become accustomed to wearing the brace. X-rays are used to assess the correction of the spine in the brace and are taken periodically (every 3–4 months) to monitor the curve. The total length of time the brace will need to be worn is dependent on the remaining spinal growth. In general, the brace is worn until spinal growth has been completed. As this point is reached, the hours spent wearing the brace will be reduced and the brace ultimately discontinued.
When is surgery needed?
The indication for proceeding with surgical treatment of scoliosis is dependent on multiple factors. The diagnosis and magnitude of the curve are the primary factors used in determining whether surgery is required to treat the deformity. Patients with idiopathic scoliosis, whose curves have progressed to greater than 40–50°, despite brace wear, are considered candidates for surgical treatment. Other important factors include the curve pattern, trunk imbalance, and skeletal maturity. The goal of surgical treatment is to provide a method for correcting the deformity, as well as preventing further progression of the curvature. Surgery is therefore useful in patients who have progressive curves that have not been controlled by brace treatment or who have curves that are too large to be amenable to brace treatment.